Oral Surgery in New Jersey

Our goal is to provide our patients with the most comprehensive, up to date treatment available in our specialty. Emphasis is placed on individualized, compassionate, and cost effective surgical care. These standards are achieved by continual upgrading and modernization of our facilities and by promoting continuing education amongst the doctors and staff. We pride ourselves in sustaining a consistent, dependable and professional working relationship between the doctors, staff and with our referring physicians. Our oral surgical care is delivered in three, convenient, well-maintained, state of the art facilities that are measured against the highest standard of excellence in the country.
A wisdom tooth that is deemed problematic is normally extracted to avoid any oral complications. To have a wisdom tooth removed, a small incision is made to open up the gum tissue over the tooth and remove any bone that is covering the tooth. Once the tooth is in view, it is gently grasped with a dental instrument, known as a forcep, and gently rocked back and forth to loosen it from the jaw bone and surrounding ligaments. Sometimes the tooth may need to be cut into smaller pieces to make it easier or removal. Stitches may be necessary after the removal of a wisdom tooth.
There are three sets of molars that erupt sequentially into our mouths beginning with the first molars (6 year molar), followed by the second molars (12 year molar) and finally the third molars, 18 year molar or the infamous wisdom teeth. “Wisdom teeth “are generally the last teeth to erupt and are the teeth least needed for good oral health. Often times they do not erupt, or emerge from your gums and remain impacted or trapped in your jawbone. If these teeth remain impacted (or buried), you may be unaware they are even present. In this position they may be the cause of any one of a number of problems. If they do erupt into your mouth the wisdom teeth may position themselves in such a position that they cause damage to your existing healthy dentition.
Common questions regarding wisdom teeth:
Why Should I Remove My Wisdom Teeth?
Wisdom teeth are the last teeth to erupt. In fact you may be aware of the phrase “6-year molar” and “12-year molar”, wisdom teeth are nothing more then “18-year molars”. They are the last set of molars to erupt and they usually erupt between the ages of 16 and 20 (around the time we allegedly attain more knowledge/wisdom). Wisdom teeth may grow sideways, partially emerge from the gum, or even remain trapped beneath the gum and bone (impacted). These poorly positioned, impacted teeth can be responsible for a wide range of problems. When they are partially erupted, the opening around the tooth allows bacteria to grow and may eventually cause a localized infection or perhaps a severe facial cellulitis.
The result: may be swelling, stiffness, pain and possible systemic illness. The pressure from the erupting wisdom tooth may move or shift your other teeth, disrupt previous orthodontic work and the natural alignment of the surrounding teeth. The most serious problems occur when tumors or cysts form around the impacted wisdom tooth, resulting in the destruction of the jawbone and otherwise healthy teeth. Removal of the offending impacted teeth will usually resolve these problems. Early prophylactic removal is recommended to avoid such problems and to decrease the surgical risk associated with the procedure.
Do all Wisdom Teeth need to be removed?
Wisdom teeth may not require removal if they are aligned properly and the surrounding gum tissue is healthy. This however is generally not the case. The removal of wisdom teeth is recommended when these teeth are prevented from properly erupting into the mouth.
When should I have my Wisdom teeth evaluated?
Whether you have obvious symptoms or not, we strongly recommend that your Wisdom teeth are evaluated between the ages of 16 and 20. If treatment is indicated, this age represents the most ideal time for surgical intervention.
As oral and maxillofacial surgeons, we are uniquely trained to manage pain and anxiety in an outpatient surgical setting. Our anesthesia training includes 9-12 months of full time, comprehensive exposure to multiple anesthetic techniques in an operating room environment. As oral surgeons we have routinely provided outpatient intravenous anesthesia for over 50 years. Many of these anesthesia techniques are now common practice and are utilized today in most outpatient surgical settings (colonoscopy, plastic procedures, etc.).
In our offices we have at our disposal a wide range of techniques and drugs that enable us to address every patient and clinical situation in a unique and customized way. For the extreme situations that may involve extensive surgery or procedures that may be complicated by significant medical histories, the facilities at Hackensack University Medical Center are utilized. Our facilities are fully equipped to assure a pain free and comfortable surgical procedure. Every patient and surgical procedure have their own unique characteristics and these are recognized by the doctors and staff during our presurgical evaluation. Local anesthesia is the most common technique used in dental offices for pain control. Based on the patient and clinical situation we may utilize any one of a number different local anesthetic agents for your surgical procedure. In addition our offices are equipped for the administration of inhalation anesthetic agents that range from nitrous oxide (laughing gas) to full inhalation general anesthetics. For many patients, intravenous medication may be required and these drugs may be used to provide conscious sedation or general anesthesia. All of our anesthetized patients are fully monitored utilizing state of the art anesthesia monitors. The doctors and staff are trained in the management of medical and anesthetic emergencies. Emergency equipment and associated drugs are regularly maintained and readily available.
In conjunction with our staff we have the ability to manage most pediatric cases in a safe, comfortable and non-threatening environment. We are aware that pediatric problems often surface without notice and these cases are given a priority during our busy day. As always, we ask for your cooperation and understanding in emergency situations.
All surgical procedures are followed by a post-operative course that we anticipate will be associated with some degree of discomfort. As we have stressed throughout our web site this discomfort and your recovery is variable from patient to patient and from surgical procedure to surgical procedure. All of our patients will receive written and verbal instructions describing recommended post-operative protocol and further specific instructions can be found on this web site if necessary. In addition, for your comfort you will receive a prescription for any one of a number of analgesic (narcotic and non-narcotic) preparations. These drugs are recognized as the most effective means for providing pain relief following your procedure. If relief is not obtained by following the recommended instructions, we would advise you to contact our office for further instructions. When taking oral pain medications there are a number of key points to consider:
- In addition to the desired effect of these drugs, keep in mind they all have various side effects. Nausea and constipation are the most prevalent.
- The medications are prescribed for use in the control of pain relief only and do not aid in the actual recovery process. We would advise the use of over the counter medications if they are effective in relieving your symptoms.
- Generally you should begin to see a decrease in your symptoms after the third post-operative day (it is important to understand that your symptoms should begin to decrease not disappear after 72 hours) If you notice your symptoms increasing in intensity after 72 hours we would advise that you contact our office.
We sincerely hope that we are able to make your surgical experience as comfortable and pain free as possible. This information is provided for your use and convenience. If you should have any further concerns or questions, we encourage you to contact our office directly.
Before treatment begins, a consultation is necessary. Planning orthognathic surgery is much like an exercise program: a physical exam helps to assess your health so you can find out what it will take to reach your goal. Our office will work closely with your orthodontist and restorative dentist to assess your teeth and facial bones. This will enable us to determine what we can do to achieve your intended goal. The pre-treatment consultation process will include a series of specific facial x-rays with x-ray analysis, clinical photographs, dental stone models (reproductions of your teeth) and coordination with your entire dental team (orthodontist and restorative dentist).
We use the most modern techniques available to determine exactly how your surgery will be approached. Using facial X-rays in combination with facial skeletal analysis, we are able to plan your surgery in a comprehensive, coordinated fashion. Our detailed diagnostic workup will help you understand the surgical process, the extent of the treatment prescribed and enable you to appreciate the benefits orthognathic surgery can provide.
Who Needs Orthognathic Surgery?
People who would benefit from orthognathic surgery include those with an improper bite or jaws that are positioned incorrectly. Jaw growth is a developmental process and in some instances they may develop at different rates. This developmental malformation may result in a host of problems that can affect function (chewing), speech, long-term oral health and physical appearance. Injuries to the jaws and birth defects can also affect jaw alignment. Orthodontics alone can correct many bite problems especially when only the teeth are involved. Orthognathic surgery may be required when the actual jaws require repositioning.
Difficulty in the following areas may indicate a need for orthognathic surgery and an evaluation may be indicated:
•difficulty in chewing, biting or swallowing
•speech problem
•chronic jaw or TMJ pain
•open bite
•protruding jaw
•breathing problems
Any of these concerns may exist at birth or may be acquired after birth as a result of hereditary influences, environmental influences or a traumatic injury to the face. Before treatment begins, a consultation is necessary. Planning orthognathic surgery is much like an exercise program: a physical exam helps to assess your health so you can find out what it will take to reach your goal. Our office will work closely with your orthodontist and restorative dentist to assess your teeth and facial bones. This will enable us to determine what we can do to achieve your intended goal. The pre-treatment consultation process will include a series of specific facial x-rays with x-ray analysis, clinical photographs, dental stone models (reproductions of your teeth) and coordination with your entire dental team (orthodontist and restorative dentist). We encourage you to ask any questions that you have regarding your treatment. When you are fully informed about every aspect of your care, you and your dental team will make the decision to proceed with treatment together.
Technology and Orthognathic Surgery
We use the most modern techniques available to determine exactly how your surgery will be approached. Using facial X-rays in combination with facial skeletal analysis, we are able to plan your surgery in a comprehensive, coordinated fashion. Our detailed diagnostic workup will help you understand the surgical process, the extent of the treatment prescribed and enable you to appreciate the benefits orthognathic surgery can provide.
Oral and Maxillofacial Surgeons are trained, skilled and uniquely qualified to manage and treat acute injuries to the facial skeleton. Drs Barbieri, Colameo and Berardo maintain active staff privileges at Hackensack University Medical Center. We are very fortunate to be an integral part of the trauma team at Hackensack University Medical Center. The Medical Center is recognized nationally for its emergency services and is a state designated Level II Trauma center. Our emergency room coverage for facial injuries includes:
- Facial lacerations
- Intra oral lacerations
- Avulsed (knocked out) teeth
- Fractured facial bones (cheek, nose, or eye socket)
- Fractured jaws (upper and lower jaw)
Injuries to the face, by their very nature, impart a high degree of emotional and physical trauma to many of our patients. The art and science of treating facial injuries requires special training involving “hands on” experience. The doctors and staff have an intimate and an understanding of how the treatment we provide will influence our patient’s long-term function and appearance.
Our emergency room coverage for facial injuries includes:
- Facial lacerations
- Intra oral lacerations
- Avulsed (knocked out) teeth
- Fractured facial bones (cheek, nose, or eye socket)
- Fractured jaws (upper and lower jaw)
Injuries to the face, by their very nature, impart a high degree of emotional and physical trauma to many of our patients. The art and science of treating facial injuries requires special training involving “hands on” experience. The doctors and staff have an intimate and an understanding of how the treatment we provide will influence our patient’s long-term function and appearance.
The Nature of Maxillofacial Trauma
There are a number of possible causes of facial trauma. Motor vehicle accidents, accidental falls, sports injuries, interpersonal violence and work related injuries. Facial injuries can range from injuries to the teeth, to extremely severe injuries of the skin and bones of the face. Typically, facial injuries are classified as soft tissue (skin and gums), bony (fractures), or injuries to special regions (such as the eyes, facial nerves or the salivary glands).
Soft Tissue Injuries of the Maxillofacial Region
When soft tissue injuries such as lacerations occur on the face, they are repaired by suturing. In addition to the obvious concern of providing primary repair which will yield the best cosmetic result possible, care must be taken to inspect for and treat injuries to specialized structures such as facial nerves, salivary glands and salivary ducts (or outflow channels for saliva).
Bone Injuries of the Maxillofacial Region
Fractures of the facial bones are treated in a manner similar to fractures in other parts of the body. The specific form of treatment is determined by various factors which include the location of the fracture, the severity of the fracture, the age and general health of the patient. When an arm or a leg is fractured, a cast is often applied to stabilize the bone to allow for proper healing. Since a cast cannot be placed on the face, other means have been developed to stabilize facial bone fractures.
One of these options involves wiring the jaws together for certain fractures of the upper and/or lower jaw. Certain types of fractures of the jaw are best treated and stabilized by the surgical placement of small plates and screws at the involved fracture site. This technique is called “rigid skeletal fixation”. The relatively recent development and use of rigid fixation has profoundly improved the recovery period for many of our patients, allowing them to return to normal function more quickly.
The treatment of facial fractures should be accomplished in a thorough and predictable manner. More importantly, the patient’s facial appearance should be minimally affected. An attempt at accessing the facial bones through the fewest incisions necessary is always considered during fracture repair. The incisions that become necessary are designed to be small and, whenever possible, are placed so that the resultant scar is minimal.
Injuries to the Teeth and Surrounding Dental Structures
Isolated injuries to teeth are common and may require the expertise of various dental specialists. Oral surgeons commonly are involved in treating fractures of the supporting bone or in re-implanting teeth which have been displaced or knocked out. These types of injuries are treated by one of a number of techniques of splinting teeth (stabilizing by wiring or bonding teeth together). If a tooth is avulsed (knocked out), it is best to have it re-implanted as soon as possible after the accident. The sooner the tooth is re-inserted into the dental socket, the better chance it will survive. If immediate replacement is not possible the tooth should be placed in salt water or milk and be subject to minimal handling. Never attempt to wipe the tooth off, since remnants of the specialized dental ligament which hold the tooth in the jaw are attached. This ligament is vital to the success of re-implanting the tooth. In the event that injured teeth cannot be saved or repaired, dental implants are often now utilized as replacements for missing teeth.
Trauma Prevention
Maxillofacial injuries, or facial trauma, refer to any injury to the mouth, face, and jaw.
In more severe cases a person may be rendered unconscious, disoriented, nauseated, dizzy or otherwise incapacitated. In these cases immediate medical attention is required and you should call 911 immediately. Do not attempt to move the individual yourself. If these symptoms are not present and the injury is severe or you are uncertain about its severity, you can contact our office. As Oral and Maxillofacial surgeons we are the specialty most suited to diagnosis and treat injuries to the teeth, mouth, jaws and facial structures.
While not all facial injuries are extensive, they are all complex since they affect an area of the body that is critical to breathing, eating, speaking and seeing. A good rule of thumb is not to take any facial injury lightly. It is virtually impossible to prevent maxillofacial injuries in today’s active society, however it is possible to protect ourselves from some of the more common causes of maxillofacial injuries and prevention with regards to oral facial injuries is always desired. We are strong advocates of the use of all protective measures available such as automobile harnesses, protective mouth guards, and appropriate masks and helmets for those who participate in athletics at any level.
Sports injuries are a leading cause of maxillofacial injuries and can be greatly reduced with the aid of a properly fitted athletic mouthguard. You don’t have to play at the professional level to sustain a serious maxillofacial injury. Make sure your family is well protected. If you participate in sports at any level, we strongly advise that you make the following safety gear a part of your standard athletic equipment:
- Football: Helmets with face guards and mouth guards should be worn. Many of the helmets manufactured for younger players have plastic face guards that can be bent back into the face and cause injury. These should be replaced by carbon steel wire guards.
- Baseball: A catcher should always wear a mask. Batting helmets with a clear molded plastic face guard are now available; these can also be worn while fielding.
- Ice Hockey: Many ice hockey players are beginning to wear cage-like face guards attached to their helmets. These are superior to the hard plastic face masks worn by some goalies, as the face guard and the helmet take the pressure of a blow instead of the face. For extra protection, both face and mouth guards — including custom mouth guards and secured with straps — should be worn.
- Wrestling: More and more high school athletic associations require wrestlers to wear head gear. A strap with a chin cup holds the gear in place and helps steady the jaw. Recently, face masks have been developed for wrestlers, who should also wear mouth guards.
- Boxing: Mouth guards are mandatory in this sport. A new pacifier-like mouth guard for boxers has been designed with a thicker front, including air holes to aid breathing.
- Lacrosse: Hard plastic helmets resembling baseball batting helmets, with wire cage face masks, are manufactured for this sport.
- Field Hockey: Oral and maxillofacial surgeons recommend that athletes participating in this sport wear mouth guards. Goalies can receive extra protection by wearing Lacrosse helmets.
- Soccer: Soccer players should wear mouth guards for protection. Oral and maxillofacial surgeons advise goalies to also wear helmets.
- Biking: All riders should wear lightweight bike helmets to protect their heads. Scooters and Skateboarders: Bike helmets are also recommended for those who ride two-wheeled scooters and skateboards.
- Skiing and Snowboarding: The recent surge in accidents among skiers and snowboarders has encouraged many safety conscious participants to wear lightweight helmets that will protect the maxillofacial area in the event of a fall or crash.
- Horseback Riding: A helmet and mouth guard are recommended for horseback riding, particularly if the rider is traveling cross-country or plans to jump the horse.
- Basketball, Water Polo, Handball, Rugby, Karate, Judo, and Gymnastics: Participants in these sports should be fitted with mouth guards.
Despite the innovations in mouth and face guard technology, many athletes continue to subject themselves to needless sports-related injuries to the mouth and face. Drs. Barbieri, Colameo & Berardo are very active in our communities in encouraging the use of oral and facial protection during athletic competition. We have taken a proactive role with our local schools in promoting their use. New synthetic materials and advances in engineering and design have resulted in mouthguards that are sturdier yet light enough to allow ease of breathing and communication during athletic competition. We recommend that oral mouthguards should be evaluated according to five very important criteria:
- Comfort and retention. They should be comfortable and retentive. It is important they cover the upper teeth and part of the gums to afford maximum protection.
- Proper fit. Mouth guards should be constructed so that they do not misalign the jaws or throw off the bite.
- Light weight. They should be light weight to allow the athlete the ability to speak and breathe
- Strong and durable. Mouth guards should be strong, durable and tear resistant
- Cleansable. Easy to maintain and clean
We encourage you to discuss this very important issue with our doctors.
Dental implants are changing the way people live. Modern implants (Osseointegrated Implants- implants bonding to bone) are designed to provide a firm foundation for the replacement of teeth. Osseointegrated implants look, feel and function like natural teeth. The person who has lost teeth may loose the ability to eat comfortably and speak confidently. This loss can have an effect on an entire personality. Fortunately osseointegrated implants can help. Drs. Barbieri, Colameo & Berardo will work closely as part of your dental implant team and with your restorative dentist to prepare your jaw for placement of the appropriate implant prosthesis. We are confident that your restoration will appear natural and your facial contours preserved.
Deciding on Dental Implants:
As you review the selected material and information throughout our website, it is important that you have the understanding of the many facets of implant dentistry. The restoration of missing teeth is not as straight forward as one might think. When a single tooth is lost there are a wide range of potential consequences that may result and if there are multiple missing teeth the consequences increase significantly. We must first realize the replacement of a missing tooth is ultimately an elective decision. After consultations and a review of appropriate information each and every patient must make the final decision on, if and when a particular tooth or teeth should be replaced. The alternatives to tooth replacement are varied and include no treatment at all, conventional dental restorations and more recently bone integrated dental implants.
Your decision to consider dental implants and reconstructive surgery may be based on any one of a number of variables. It is always in your best interest to have an experienced surgeon provide you with an explanation of exactly what is involved in your specific case. In today’s crowded market place many types of facilities are providing access to dental implants. Many of these offices advertise attractive surgical fees, all services provided under one roof and other superficially attractive options such as “teeth in a day”.
The following points should be noted and may be critical in your decision to move ahead with surgical treatment:
- It should first be emphasized that in spite of what is advertised the only trained specialists in the surgical placement of osseointegrated implants are Oral and Maxillofacial Surgeons and our periodontal colleagues (Periodontists). There simply is no other trained surgical specialist recognized by the American Dental Association in the placement of dental implants.
- The next important issue is the need for careful pre-operative evaluation and preparation, immediate post-operative follow-up and ultimately, long term follow-up. Comprehensive surgical care that is required for implant reconstructive surgery can only be provided by a trained, qualified and full time surgical practice. One should be careful when committing to a large “group dental practice” facility or even a smaller dental practice that may provide the expertise of some type of surgeon on a limited part time basis. Keep in mind that in our office you will always be examined and treated by a Board Certified Oral and Maxillofacial Surgeon, 100% of the time. Our full time surgical practice provides you with full coverage of any potential complication 24 hours/day, 365 days/year. Furthermore we have full hospital privileges and access to the emergency room and operating room at Hackensack University Medical Center if the need should ever arise
- The last important point to be aware of is the surgical fee. Our surgical fee includes the use of only top quality, rigidly controlled bone replacement and dental implant products. There are many dental implant companies recognized in the United States and suffice to say all dental implants are NOT equal! Our office has been placing Osseointegrated implants for over 25 years and we are committed to a one of the original dental implant companies, Zimmer, Inc. Zimmer, Inc. has been in the business of making body parts for over 50 years and is well known throughout the industry. As a bioengineering company they are world renowned for innovations in the growing field of bio-mechanics and bio-engineering. There systems are supported by a rigorous research, development, product management and field support that is unprecedented in their industry.
If you would desire additional information and explanations regarding dental implants and oral reconstructive surgery we would invite you to view the video presentations provided throughout our web site.
What are Dental Implants?
The implants themselves are titanium posts that are inserted into the jawbone where teeth are missing. These metal anchors act as tooth-root substitutes. They are surgically placed into the jawbone and the bone bonds (osseointegrates) directly with the titanium, creating a strong foundation for artificial teeth. Small posts are then attached to the implants that protrude through the gums. These posts will provide stable anchors for artificial replacement of your teeth. Implants will also help to preserve the facial structure and prevent bone deterioration that normally occurs when teeth are lost.
The Surgical Procedure
The placement of dental implants is a surgical procedure, with all the attendant risks, benefits and alternatives associated with any surgery. For most patients, the placement of dental implants will involve two surgical procedures. During first stage surgery, implants are placed within your jawbone. For three to six months following your first stage surgery, the implants are beneath the surface of the gums gradually bonding (osseointegration) with the jawbone. You should be able to wear your temporary dentures and eat a soft diet throughout this healing phase. During the osseointegration phase your dentist will be planning for the final prosthetic replacement of your teeth.
There is much discussion today about “immediate implants”. This concept involves either:
- The removal of a tooth and the immediate placement with an implant
- The placement of an implant with the immediate placement of a functional restoration.
While this type of treatment on occasion is possible, it is not the standard of care, and most times is contra-indicated. During the consultation and treatment-planning phase of your treatment, this concept may be discussed if it pertains to your case. It is our philosophy and goal to optimize our surgical procedure in an effort to provide you with the very best chance of a successful outcome. Our surgical recommendations are always based on sound, well-researched biological principals that are uncompromising.
After the implants have integrated (bonded) to your jawbone, the second phase of treatment begins. The doctors will uncover the implants and attach small posts that will act as anchors for the artificial teeth. These posts protrude through the gums. Once the artificial teeth are placed these posts will not be seen. The entire procedure may take up to six months. The doctors will work very closely as part of your restorative team to ensure that your implant experience will have a minimal impact on your daily routine.
How can I access additional information on Dental Implants?
Additional information on Dental Implants is readily available through the specific web link to the American Association of Oral and Maxillofacial Surgeons at: http://www.aaoms.org/dental_implants.php
Major and minor bone grafting
A jaw bone (maxilla/mandible) that is without teeth for an extended period of time will gradually resorb and atrophy (disintegrate or wash away). This often results in a condition in which there is poor quality and quantity of bone suitable for placement of dental implants. In most cases where osseointegrated implants are being considered the limiting factor is the amount of bone available to place the implants. The amount of bone may be deficient in either a vertical or horizontal dimension. This lack of viable bone will necessitate a bone grafting procedure to restore the anatomy and allow for proper prosthetic treatment.
We now have the ability to graft autogenous (bone harvested form the same patient) bone when indicated. This gives us the opportunity to place implants of proper length and width, but more importantly it provides the ability to restore proper function and aesthetics.
Depending upon the specific requirements of each patient’s case, bone-grafting procedures may be performed separately or on occasion simultaneously with the placement of osseointegrated implants. There are several areas of the body that are suitable for obtaining bone grafts. In the maxillofacial region, bone grafts can be taken from inside the mouth, in the area of the chin, third molar region or in the upper jaw behind the last tooth. In more extreme cases, a greater quantity of bone may be required and this can be obtained from the hip or the outer aspect of the knee.
Many of these procedures are performed in our office on a daily basis, often with the aid of IV sedation or general anesthesia. In more complex instances the doctors may elect to admit the patient to Hackensack University Medical Center. There are many types of bone grafting techniques and the following is a brief list of some of the procedures that we perform. These techniques are all case specific depending on the many variables that go into to coordinating your case.
Sinus lift procedure
This procedure involves surgery above the maxillary posterior teeth. During this procedure we elevate the maxillary sinus membrane and place a bone graft that is harvested from another site in the mouth, onto the sinus floor. This will increase the amount of bone available for implants in a vertical direction and allow implants to be placed in the back part of the upper jaw.
Ridge-augmentation
In severe cases the alveolar ridge (the alveolar ridge is the portion of bone in our mouths that generally supports the teeth) is reabsorbed and a bone graft is necessary to increase the ridge height and/or width to accommodate an osseointegrated implant. This procedure involves grafting autogenous bone (bone from the same person’s body) to the desired location in the mouth.
Nerve- repositioning
When considering implants in the lower jaw, the inferior alveolar nerve, which gives feeling to the lower lip and chin, may restrict the quantity of bone available to place implants in the posterior aspect of the mandible. We now have the ability to reposition this rather large sensory nerve in order to make room for placement of dental implants to the lower jaw.
Immediate Extraction Socket Graft
Often times an osseointegrated implant is considered as the replacement of choice for an extracted tooth. It may be advantageous to immediately fill the missing tooth socket with an artificial bone substitute to properly prepare the extraction site for ideal implant placement.
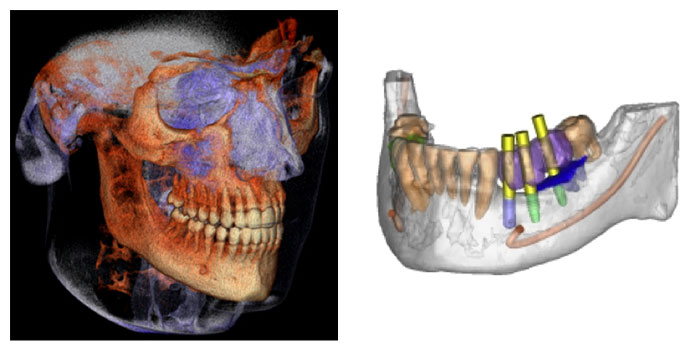
Currently our offices are 75% digitalized and we are equipped to perform the following film studies within the confines of our offices:
- Periapical radiograph: This x-ray is the conventional dental radiograph (small dental radiographs) and is used in our office on occasion.
- Orthopantomogram (Panorex): Panoramic imaging remains the standard of care for many types of dental procedures. In todays medical world the panorex is without question the most comprehensive preliminary screening imaging study available. It is essential for almost any type of oral surgical procedure. This study provides us with a complete over view of the lower 1/3 of the facial skeleton provides an enormous amount of diagnostic information with minimum radiation exposure. It remains the back bone of oral surgery and the least invasive (with respect to radiation exposure and patient acceptance). Panoramic units are in place at all three office locations and are of the highest quality, emitting the least amount of radiation while providing us with the necessary diagnostic information.
- Our most recent advancement is our Cone Beam Computerized Tomographic (CBCT) machine located in the Hackensack office. This unit is a Kodak 9300CT and can provide a fully digitized 3-D study of the entire facial skeleton. The Kodak 9300CT is the most sophisticated cone beam unit available on todays market and while these units are becoming popular, there are a number of distinguishing features about our unit which make it the most sophisticated unit available at this time:
- The lowest level of radiation emissions per study.
- The 9300CT enables us to isolate our study, if necessary, to a small area of interest rather than “shoot the whole face”. From our point of view this feature is critical with respect to our patients overall health and welfare as we are able to effectively minimize radiation exposure to our patients and scan small isolated areas throughout the facial skeleton when necessary.
This new addition to our diagnostic armamentarium provides us with cutting edge technology that enables us to provide a clear and more definitive diagnosis (especially with respect to implant restoration and facial reconstruction) and more accurately anticipate potential surgical sequel.
The Carestream 9300CT is the most sophisticated cone beam unit available on today’s market and while these units are becoming popular, there are a number of distinguishing features about our unit which make it the most sophisticated unit available at this time:
- The lowest level of radiation emissions per study. Your health and safety is our greatest concern.
- The 9300CT enables us to isolate our study, if necessary, to a small area of interest rather than “shoot the whole face”. From our point of view this feature is critical with respect to our patients overall health and welfare as, once again we are able to effectively minimize radiation exposure to our patients and scan small isolated areas throughout the facial skeleton when necessary
- High resolution images that allow us to see your teeth and facial skeleton with unprecedented detail
- Comfortable positioning: the system’s open design makes exams more comfortable, with both seated and standing options to accommodate patients of all sizes and the unit is wheelchair accessible
- Improved care: we can perform a wider range of diagnoses with even greater accuracy
The new addition of this versatile 3D system to our diagnostic armamentarium provides us with cutting edge technology. You will see this “cutting edge technology” is evident throughout all aspects of our practice and it allows us to meet the full range of our patients imaging needs. In addition to the 3D images, this 3-dimensional system will also deliver crystal clear 2D panoramic radiographs (conventional x-rays), which still form the diagnostic foundation of most cases. These images enable us to provide a clear and more definitive diagnosis (especially with respect to implant restoration and facial reconstruction) and more accurately anticipate potential surgical sequela. Because many cases require additional anatomical detail, the system’s multiple 3D imaging capabilities support a wide range of clinical applications with focused-field, single and dual jaw views. TMJ, sinus and maxillofacial views are easily obtainable. This state-of-the-art technology will help us diagnose with an enhanced level of accuracy and provide treatment with unprecedented confidence. Whether we are analyzing a complex tooth impaction, planning a multi-site implant case, or visualizing TMJ dysfunction, the precise, crystal-clear 3D and panoramic images will help us to formulate a specific treatment plan that will address your needs and answer any questions that you may have about your care and treatment options.
This new addition to our diagnostic armamentarium provides us with cutting edge technology that enables us to provide a clear and more definitive diagnosis (especially with respect to implant restoration and facial reconstruction) and more accurately anticipate potential surgical sequel.
Our office is proud to provide our patients with “cutting edge” developing technologies that accelerate the healing process in the most natural way possible. It is a consistent goal throughout our practice to improve our surgical technique and predictably provide our patients with the very best results possible. We accomplish these goals through additional continuing education and taking advantage of the latest in what the rapidly advancing Biotechnical industry has to offer.
The latest advancement involves understanding how our own body’s natural growth factors help to accelerate the healing process and is currently being applied in our oral reconstruction procedures. The technique involves the use of very specific healing factors found in our blood stream and more specifically in our blood cells or platelets.
Platelet Rich Plasma (PRP) is a volume of autogenous (your own) plasma that has a platelet concentrate above the body’s normal baseline. Normal platelet concentrates in the blood range from 150,000 to 350,000. Today, scientific proof has unequivocally demonstrated dramatically enhanced bone and soft tissue healing using Platelet Rich Plasma with concentrations of 1,000,000. Until now, the use of PRP has been confined to the hospital setting. This was due mainly to the cost of separating the platelets from the blood and the large amount of blood needed to produce a suitable quantity of platelets. Our office now possesses the technology to harvest, process, concentrate and deliver these growth factors directly to our operative sites. This technique represents the latest in bio-tissue engineering and cellular therapy and has been perfected over the past 10 years. Now with the help of Harvest Technologies Corporation our office can harvest and produce a high quality concentrate of platelets from blood drawn directly from our patients while they are undergoing outpatient surgery.
Why all the excitement about Platelet Rich Plasma (PRP or more specifically Autogenous Platelet Concentrate, and we emphasize autogenous which refers to your own)?
PRP permits the body to take advantage of the normal healing pathways at a greatly accelerated rate. During the healing process, the body rushes many cells and cell-types to the surgical site in order to initiate the healing process. One of those cell types is platelets. Platelets are carriers of proteins specifically involved in regeneration of injured tissues; these proteins are termed Growth Factors. Platelets perform many functions, including formation of a blood clot and ultimately the release of growth factors (GF) into the wound. The GF (platelet derived growth factors PGDF, transforming growth factor beta TGF, vascular endothelial growth factor, epithelial growth factor and insulin-like growth factor ILGF) function to assist the body in repairing itself by stimulating stem cells to regenerate new tissue. The more growth factors sequestered and released into the wound, the more stem cells stimulated to produce new host tissue. Thus, it has been demonstrated that PRP permits the body to heal more rapidly and more efficiently.
One of the aforementioned growth factors TGF, contains a sub-family of growth factors that is valuable in our bone grafting procedures. This factor is bone morphogenic protein (BMP) and it has been shown to induce the formation of new bone when concentrated around living bone cells (osteoblasts). This is of great significance when it is used in conjunction with the placement of dental implants. By adding PRP, and thus BMP, to the implant site with autogenous (your own) bone cells, we can grow bone more predictably and faster than ever before. This enables us to place implants in areas of the mouth that may not have been previously possible!
Platelet Rich Plasma has many clinical applications:
- Bone grafting for dental implants. This includes onlay and inlay grafts, sinus lift procedures, ridge augmentation procedures, and closure of cleft lip and palate defects.
- Repair of bone defects created by removal of teeth or small cysts
- Repair of fistulas between the sinus cavity and mouth
Platelet Rich Plasma has many advantages:
- Safety: PRP is a by-product of our patient’s own blood; therefore, disease transmission is not an issue.
- Convenience: PRP is processed in our office, under strict sterile conditions, simultaneously while the patient is undergoing an outpatient surgical procedure, such as placement of dental implants. The patients own blood is removed at the time of preparation of the IV site for general anesthesia.
- Faster healing: The super saturation of the wound with PRP, and the described growth factors, produces an increase of tissue synthesis and thus faster tissue regeneration.
- Cost effectiveness: Since PRP harvesting is performed with only a small portion of blood in the doctor’s office, the patient need not incur the expense of the harvesting procedure in the hospital or at the blood bank.
Frequently asked questions about PRP:
- Is PRP safe? Yes. During the outpatient surgical procedure a small amount of your own blood is drawn out via the IV. This blood is then placed in a specially designed centrifuge machine (Harvest Technologies Corporation) and processed under the strictest guidelines. In less than fifteen minutes, the Platelet Rich Plasma is formed and ready to use.
- How long has PRP been in use? As a hospital adjunctive procedure, application of PRP has been in use for about a decade by Oral Surgeons, Plastic Surgeons, Orthopedic Surgeons and Cardiovascular Surgeons.
- Why hasn’t it been used in an office sooner? Until recently the technology to properly produce the concentrate was not available in private practice. The process was complex, time consuming, expensive, and required large volumes of the patient’s blood. It involved outside personnel and the transfusion of blood products. Furthermore, through research we have discovered that it is not enough to merely concentrate platelets but equally as important, we must concentrate them and produce a quality concentrate. Normal centrifugation will concentrate platelets but it destroys the integrity of the platelets rendering them useless.
- How then is the PRP produced in your office? At the same time we begin our general anesthesia IV line we withdraw a small portion of your own blood. This blood is then processed in a specialized centrifuge (designed by Harvest Technologies Corporation) that spins and automatically separates the red blood cells from the plasma. Then, using a double centrifuge technique the plasma is further processed and an autologous platelet concentrate and its effective growth factors are produced. The entire process takes only 15 minutes and is completed simultaneously while we are treating you surgically!
- Can PRP be used alone to stimulate bone formation? No. PRP must be mixed with your own bone for the most beneficial effects
- Are there any contraindications to PRP? Very few, patients with bleeding disorders or hematologic diseases do not qualify for this in-office procedure.
The inside of the mouth is normally lined with a special type of skin (mucosa) that is smooth and coral pink in color. Any alteration in this appearance could be a warning sign for a pathological process. The most serious of these is oral cancer. The following can be signs of the beginning of a pathologic process or cancerous growth:
- Reddish patches (erythroplasia) or whitish patches (leukoplakia) in the mouth
- A sore that fails to heal and bleeds easily
- A lump or thickening on the skin lining the inside of the mouth
- Chronic sore throat or hoarseness
- Difficulty in chewing or swallowing
These changes can be detected on the lips, cheeks, palate, gum tissue around the teeth, tongue, face and neck. Pain does not always occur with pathology, and curiously, is not often associated with oral cancer. However, any patient with persistent facial and/or oral pain without an obvious cause or reason may also be at risk for oral cancer.
We would recommend performing an oral cancer self-examination monthly and remember that your mouth is one of your body’s most important warning systems. Do not ignore suspicious lumps or sores. Please contact our office, we can be of some help.
TMJ (temporomandibular joint) disorders represent a family of problems related to your complex jaw joint. If you have had symptoms like pain or a “clicking” sound in the area of your “jaw hinge”, you will be glad to know that these problems are now more easily diagnosed and treated than they were in the past. If you are considering treatment for TMJ in North Bergen, Hackensack or Ridgefield, NJ, please call our office to schedule a consultation so that we may better answer your questions about the process.
Since some types of TMJ problems can lead to more serious conditions, early detection and treatment is important. No one treatment can resolve TMJ disorders completely and most treatment modalities will take time to be effective.
What is the TMJ?
The temporomandibular joint, better known as the TMJ, is the small joint located in front of the ear where the skull and the jawbone connect. The TMJ is composed of a “ball” (the condyle), “socket” (articular fossa), and interfacing tissue between the ball and the socket known as the articular disc (cartilage). This disc is made from strong, white cartilaginous tissue that does not have nerves or a blood supply. It prevents the two bones of the joint from touching each other (provides a cushion effect), thus avoiding wear on the bones themselves. At the rear of the joint, the articular disc (cartilage) attaches to the bilaminar zone (posterior disc attachment), which does contain nerves and blood vessels and can be quite sensitive. The front end of the disc is connected to a muscle that is attached to the condyle. This is the external pterygoid muscle that helps to open the mouth.
Trouble with Your Jaw?
TMJ disorders may develop for many reasons. You might clench or grind your teeth, tightening your jaw muscles and stressing your TM joint. You may have a damaged jaw joint due to an injury or disease. Whatever the cause, the results may include a misaligned bite, pain, clicking, grating noise when you open your mouth or difficulty in opening your mouth wide.
Do You Have a TMJ Disorder?
- Are you aware of grinding or clenching your teeth?
- Do you wake up with sore, stiff muscles around your jaws?
- Do you have frequent headaches or neck aches?
- Does the pain get worse when you clench your teeth?
- Does stress make your clenching and pain worse
- Does your jaw click, pop, grate, catch, or lock when you open your mouth?
- Is it difficult or painful to open your mouth, eat or yawn?
- Have you ever injured your neck, head or jaws
- Have you had problems (such as arthritis) with other joints?
- Do you have teeth that no longer touch when you bite?
- Is it hard to use your front teeth to bite or tear food?
- Are your teeth sensitive, loose, broken or worn?
The more times you answered “yes,” the more likely it is that you have a TMJ disorder. Understanding TMJ disorders will also help you understand how they are treated.
Diagnosis of TMJ Disorders
Diagnosis of TMJ disorders generally involves obtaining a comprehensive medical history, review of complaints and clinical examination. Generally x-rays of the jaws and jaw joints are obtained in the office. If more advanced imaging studies such as CT scans or MRI studies are required, appropriate referrals will be made directly through our office.
Treatment
- There are various treatment options available:
- Anti-inflammatory and muscle relaxing medications
- Physical therapy including ultrasound and electrical stimulation
- Oral appliances (bite plates)
- Biofeedback therapy
- Various surgical procedures
What Causes Snoring?
During sleep, the muscles and the soft tissues in the throat and mouth relax, constricting the airway. This increases the velocity of air flowing through the airway. As the air velocity is increased in the constricted space, soft tissues like the soft palate and the uvula vibrate, resulting in snoring. Excess body weight, heavy alcohol consumption and other sedative medications have been shown to increase the severity of snoring.
What Is Sleep Apnea?
Sleep apnea is a common disorder that affects millions of adults. It is often undiagnosed, despite the potentially serious consequences of the disorder and it is estimated that at least ten million Americans have unrecognized sleep apnea.
Obstructive sleep apnea affects all age groups. Roughly, 40 million Americans are chronically ill with various sleep disorders, and 20-30 million Americans experience intermittent sleep-related problems. Falling asleep at the wheel of an automobile is possibly the most costly and devastating problem on America’s highways. Accidents in the workplace due to sleep deprivation are not at all uncommon. Fifty-one per cent of the American workforce report that sleepiness on the job interferes with the amount of work they achieve and two-thirds of adults report that sleepiness makes concentrating and handling stress on the job more difficult.
Diagnosis of Sleep Apnea
Sleep Apnea is a medical condition that is usually diagnosed utilizing a comprehensive history, clinical examination and a sleep study. A sleep study is usually performed at a sleep center. Our office is affiliated with the Institute for Sleep-Wake Disorders at Hackensack University Medical Center in Hackensack, New Jersey.
Treatment of Obstructive Sleep Apnea and Snoring
Obstructive sleep apnea and excessive snoring can be treated by various treatment modalities, which include the use of a CPAP (continuous positive airway pressure) machine during sleep, oral appliances and surgery. All treatment is focused on opening the airway passage in the back of the throat. The most conservative approach is the use of on oral appliance.
What are Oral Appliances?
Oral appliances come in varying designs and types and have been used in dentistry for many years for different purposes. Appliances used for the management of snoring and sleep apnea are similar in design to orthodontic appliances or athletic mouth guards. These appliances are designed to move the lower jaw into a more forward position thereby opening the restricted airway.
How Do Oral Appliances Work?
Oral appliances developed for the treatment of snoring and obstructive sleep apnea are worn in the mouth during sleep. These appliances aid in preventing the oropharyngeal tissues and the base of the tongue from collapsing and obstructing the airway. When the mandible is moved forward into a comfortable position, the tongue is automatically moved out of the airway. This can reduce snoring and help to control Obstructive Sleep Apnea.
Distraction osteogenesis (DO) is a relatively new method of treatment for selected deformities and defects of the oral and facial skeleton. It was first used in 1903. Then, in the 1950’s, a Russian orthopedic surgeon, Dr. Gabriel Llizarov slowly perfected the surgical and postoperative management of distraction osteogenesis treatment to correct deformities and repair defects of the arms and legs. His work went largely unnoticed until it was presented to the Western Medical Society in the mid-1960’s.
Distraction osteogenesis was initially used to treat defects of the oral and facial region in 1990. Since then, the surgical and technological advances made in the field of distraction osteogenesis have provided oral and maxillofacial surgeons with a safe and predictable method to treat selected deformities of the oral and facial skeleton.
The doctors use distraction osteogenesis to treat selected deformities and defects of the oral and facial skeleton. If you have questions about distraction osteogenesis, please contact our office to schedule an appointment for further discussion.
Frequently Asked Questions About Distraction Osteogenesis:
What does the term distraction osteogenesis mean? Simply stated, distraction osteogenesis means the slow movement apart (distraction) of two bony segments in a manner such that new bone is allowed to fill in the gap created by the separating bony segments.
Is the surgery for distraction osteogenesis more involved than “traditional surgery” for a similar procedure? Not usually, Distraction osteogenesis surgery is commomly performed on an outpatient basis with most of the patients going home the same day of surgery. The surgical procedure itself is less invasive so there is usually less pain and swelling.
Will my insurance company cover the cost of osteogenesis surgical procedure? Most insurance companies will cover the cost of the osteogenesis surgical procedure provided that there is adequate and accurate documentation of the patient’s condition. Of course, individual benefits within any insurance companies policy may vary. After you are examined for your consultation, we will be able to assist you in determining whether or not your insurance company will cover a particular surgical procedure.
Is distraction osteogenesis painful? Since all distraction osteogenesis surgical procedures are performed while the patient is under general anesthesia, pain during the surgical procedure is not an issue. Postoperatively, you will be supplied with appropriate analgesics (pain killers) to keep you comfortable, and antibiotics to fight off infection. Activation of the distraction device to slowly separate the bones may cause some patients mild discomfort. In general, the slow movement of bony segments produces discomfort that is analogous to having orthodontic braces tightened.
What are the benefits of distraction osteogenesis versus traditional surgery for a similar condition? Distraction osteogenesis typically produces less pain and swelling than the traditional surgical procedure for a similar condition. Distraction osteogenesis eliminates the need for bone grafts, and therefore, another surgical site. Lastly, distraction osteogenesis is associated with greater stability when used in major cases where significant movement of bony segments is involved.
What are the disadvantages of distraction osteogenesis? Distraction osteogenesis requires the patient to return to the surgeon’s office frequently during the initial two weeks after surgery. This is necessary because in this time frame the surgeon will need to closely monitor the patient for any infection and teach the patient how to activate the appliance.
Does distraction osteogensis involve additional surgery? In some cases, a second minor surgical procedure is necessary to remove the distraction appliance.
Can distraction osteogenesis be used instead of bone grafts to add bone to my jaws? Yes. Recent advances in technology have provided the oral and maxillofacial surgeon with a distraction device that can be used to slowly grow bone in selected areas of bone loss that has occurred in the upper and lower jaws. The newly formed bone can then serve as an excellent foundation for dental implants.
Does distraction osteogenesis leave scars on the face? No. The entire surgery is done within the mouth and the distraction devices used by the doctors remain inside the mouth. There are no facial surgical incisions, so no unsightly facial scars will result.
Are there any age limitations for patients who can receive osteogenesis? No. Distraction osteogenesis works well on patients of all ages. In general, the younger the patient the shorter the distraction time and the faster the consolidation phase. Adults require slightly longer period of distraction and consolidation because the bone regenerative capabilities are slightly slower than those of adolescence or infants.